Quelles sont les utilisations cliniques de l’acide hyaluronique?
The unique physical Et en pluschemical properties Et en plusmultiple physiological functions De laAcide hyaluroniquehave found widespread application dansmedicine Et en plusbiomaterials....... In Le conseil des ministres1960s, Balazs [1] first used hyaluroniqueacidein complex retinal detachment surgery, achieving significant therapeutic effects; in Le conseil des ministres1970s, hyaluronic acid preparations began À propos debe applied in joint diseases; in the 1980s, hyaluronic acid emerged in the field De laaesthetics. Since then, hyaluronic acid has been increasingly applied in ophthalmology, orthopaedics, dermatology, cosmetic surgery, and other chirurgicalefields, avecrapid advancements in related research.
1 propriétés physiques et chimiques et effets physiologiques
In 1934, Professors Meyer and Palmer from the Department De laOphthalmology at ColumbiA aUniversity in the United States first isolated hyaluronic acid (HA) from the vitreous humour De lacow eyes. In 1937, Kendell and others extracted this active substance from bacteria [2]. In 1950, Karl Meyer&#Le laboratoire a réussi à élucider la structure chimique de l’acide hyaluronique [3]. L’acide hyaluronique est un polymère de poids moléculaire élevé, dont les unités structurelles de base sont l’acide d-glucuronique et la n-acétyl-d-glucosamine, liés par des liaisons glycosidiques β-1,3 et β-1,4 alternées. En raison de la présence de groupes carboxyliques acides, l’acide hyaluronique se dissocie facilement dans une solution de chlorure de sodium, libérant H+ et adoptant un état de cation polyionique acide [4], conférant ainsi ses propriétés mucopolysaccharidiques acides.
hyaluroniqueacid is widely distributed in the connective tissues De laliving organisms, such as the umbilical cord, cartilage, vitreous humour De lathe eye, blood vessel walls, joint fluid, and skin [5] [traduction]. In biological organisms, hyaluronic acid exhibits various physiological activities, including lubricating joints, regulating protein activity, inhibiting microbial invasion and the spread of toxic substances, promoting wound healing, and regulating vascular wall permeability [6] [traduction].
2 Applications cliniques en chirurgie
2.1 traitement des maladies articulaires
Hyaluronic acid is commonly found in synovial fluid in the form of Le sodiumsalts, with Hyaluronate de sodiumbeing the primary component of synovial fluid and also a component of cartilage matrix [7]. It plays a lubricating role within the joint cavity, reducing friction between connective tissues; simultaneously, it exerts elastic properties to cushion external forces exerted on joint cartilage. Injecting high-molecular-weight, high-concentration, and high-viscoelastic sodium hyaluronateinto the joint cavity can enhance the viscosity and lubricating function of synovial fluid, protect joint cartilage from further damage, and promote the healing and regeneration of joint cartilage, significantly alleviating pain and improving joint mobility [8] [traduction].
Knee osteoarthritis: Le Bannuruet al. [9] [traduction] published a Revue systématiquein 2011, which included 54 high-quality clinical randomisécontrôléLes essais(RCTs) involving 7,545 participants. The trial design compared hyaluronic acid with placebo pourthe treatment of knee osteoarthritis, administered via intra-articular injection, with the primary outcome being the reduction in pain response. Meta-analysis results showed that treatment began to show efficacy après4 weeks, reached maximum effect after 8 weeks, and the pain-relieving effect of hyaluronic acid persisted after 24 weeks. It was concluded that hyaluronic acid can serve as an effective drug pourthe treatment of knee osteoarthritis.
Temporomandibular joint disorders: Manfrediniet al. [10] [traduction] conducted a systematic review of hyaluronic acid treatment for temporomandibular joint disorders in 2010, including 19 clinical trials, of which 12 were for temporomandibular joint disorders and 7 for temporomandibular joint arthritis. The results showed that local injection of hyaluronic acid twice weekly significantly reduced pain compared with the placebo group, while joint function and mobility improved, but there was no difference in mouth opening size between the two groups; hyaluronic acid combined with aspiration was more effective than aspiration alone; and injection of hyaluronic acid in the lower part of the joint was more effective than in the upper part.

Ankle joint diseases: Loveday et al. [11] conducted a Cochrane systematic review on the intra-articular injection of hyaluronic acid for the treatment of ankle arthritis. This étudeincluded only one clinical trial with 15 participants, with a follow-up period of 6 months. All participants underwent arthroscopic minimally invasive surgery, followed by intra-articular injection of hyaluronic acid three weeks later. The results showed that hyaluronic acid did not have a significant advantage in pain relief but improved ankle joint mobility.
Shoulder joint diseases: Saito et al. [12] [en] conducted a systematic review in 2010 on the efficacy and La sécuritéof hyaluronic acid shoulder injections for chroniqueshoulder pain. A total of 19 RCTs and 2,120 participants were included. The results showed that hyaluronic acid injections into the shoulder effectively alleviated chronic shoulder pain and improved shoulder joint function, with no significant difference in the total number of adverse reactions between the two groups. This study also conducted a subgroup analysis comparing hyaluronic acid with corticosteroids, which showed that the hyaluronic acid group had better recovery of shoulder joint function than the corticosteroid group.
2.2. - Pour la réparation des plaies
L’acide hyaluronique est l’un des principaux composants de la matrice extracellulaire de l’épiderme et du derme de la peau humaine [13] [en]. Il améliore les conditions de croissance des cellules de la peau et fournit un environnement externe optimal pour la synthèse de collagène et de fibres élastiques dans les cellules cutanées [14] [traduction]. Il protège également les cellules des tissus endommagés contre les bactéries pathogènes, réduit les réponses inflammatoires [15] [traduction], améliore la cicatrisation et la régénération des plaies, et accélère la régénération des tissus de la peau.
Trauma repair: Voigt et al. [16] conducted a systematic review and meta-analysis of hyaluronic acid treatment for trauma in 2012. This study included 10 RCTs, 4 of which involved hyaluronic acid treatment for burns and 6 for ulcerated wounds. The results showed that hyaluronic acid accelerated wound healing in burn patients, shortened healing time, and higher concentrations of hyaluronic acid formulations were more beneficial for burn repair.

Postoperative wound repair: Metwallyet al. [17] [traduction] published a systematic review in 2007 on the use of hyaluronic acid solutions to prevent postoperative adhésionsafter gynaecological surgery, including 4 RCTs. The results showed that the incidence of adhesions was lower in the hyaluronic acid group than in the control group after gynaecological surgery; in Les patientswho had developed adhesions, hyaluronic acid reduced the incidence of further adhesion progression, but there was no difference in the improvement rate of adhesions between the two groups. À propos de nouset al. [18] [traduction] published a systematic review in 2012, including five RCTs. The meta-analysis results showed that cross-linked hyaluronic acid Le gelreduces the incidence of adhesions after gynaecological surgery; in laparoscopic myomectomy, hyaluronic acid reduces the incidence of adhesions between the wound and the peritoneum; and in hysteroscopic gynaecological surgery, hyaluronic acid reduces the incidence of adhesions between the wound and the uterus.
2.3. - Pour les affections de la peau
Hyaluronic acid is the most effective natural moisturising agent discovered to date, possessing powerful water-binding and moisturising properties, capable of absorbing approximately 1,000 times its own weight in water. With age, nutritional deficiencies, sun exposure, environmental stressors, and other factors, the body's ability to synthesise hyaluronic acid gradually decreases, leading to a reduction in its concentration in the skin. This ultimately results in keratinisation, wrinkles, ageing, and even inflammatory reactions in the skin.
Actinic keratosis: Guptaet al. [19] [traduction] published a systematic review in 2012, conducting a meta-analysis of various treatment measures for actinic keratosis. The study included three randomised controlled trials (RCTs) on hyaluronic acid treatment for actinic keratosis. The intervention in the treatment group was a 3% diclofenac sodium solution containing 2.5% hyaluronic acid, while the control group received a placebo. A total of 420 participants were included. The results showed that the efficacy rate in the treatment group was higher than that in the control group.
Les rayonnementsdermatitis: Kirova et al. [20] conducted a La phaseIII. Le droit de la familleclinical trial En utilisanta randomised controlled blinded method to investigate the effect of hyaluronic acid on radiation dermatitis following radiotherapy for chest tumours. A total of 200 participants were included, with the intervention group receiving hyaluronic acid ointment and the control group receiving traditional moisturising ointment. The results showed that the incidence of radiation dermatitis was not significantly different between the two groups; however, the skin colour at the radiation site was better in the experimental group than in the control group. Additionally, the pain response in patients with radiation dermatitis was reduced after using hyaluronic acid cream. Pinnix et al. [21] conducted a randomised controlled clinical trial involving 130 participants. They compared the effects of hyaluronic acid gel and vaseline gel on the skin at the radiation site in female seinLe cancerpatients undergoing radiotherapy. Applied hyaluronic acid gel versus vaseline gel to the irradiated areas. Results showed that hyaluronic acid did not reduce the incidence of grade 2 or higher radiation dermatitis.

Scleroderma: Yu Chunshui et al. [22] [en] investigated the treatment of advanced localized scleroderma, enrolling 22 patients with scleroderma. Participants were randomly assigned to two groups: the experimental group (11 patients) received hyaluronic acid spot injections once every 5 weeks for a total of 15 weeks, while the control group (11 patients) received hyaluronic acid spot injections once weekly for a total of 15 weeks. At the end of week 15, the efficacy rate in the experimental group was 90.91%, while in the control group it was 45.45%. One adverse reActions à entreprendreoccurred in the experimental group and three in the control group, all manifesting as swelling at the injection site. The results indicate that hyaluronic acid is safer and more effective than hyaluronidase for the treatment of scleroderma.
Skin rejuvenation: Narins et al. [23] [en] selected 138 middle-aged and elderly female patients and conducted a comparative study on the efficacy of hyaluronic acid and collagen protein subcutaneous injections for the removal of nasolabial folds. The injection frequency was once every 2 weeks until the nasolabial folds faded to a satisfactory effect, with a maximum treatment duration of 6 months. The results showed that after 6 months, the efficacy rate for fading nasolabial folds was 59.6% in the hyaluronic acid group and 9.5% in the collagen group; among those who achieved satisfactory results, the number of injections required was fewer in the hyaluronic acid group than in the collagen group; there were no significant differences in post-injection reactions or tolerability between the two groups.
2.4. - Applications dans les maladies ophtalmiques
Sodium hyaluronate is an important component of aqueous humour and vitreous humour, protecting the corneal endothelium, iris, and retina [24] [traduction]. Injection of sodium hyaluronate into the anterior chamber maintains anterior chamber depth; injection into the vitreous cavity aids in retinal repositioning; and in ophthalmic surgery, it reduces intraoperative or postoperative adhesions. Hyaluronic acid can also adsorb and bind large amounts of water molecules, preventing ocular dryness, and is used for corneal damage caused by or associated with dry oeilsyndrome, intrinsic disorders, or external stimuli [25] [traduction].
Dry eye disease: mcdonald’Set al. [26] [en] selected 39 patients with dry eye disease and conducted a randomised crossover controlled trial to comparerthe therapeutic effects De 0,1%sodium hyaluronate and polyvinyl alcohol. A total of 32 patients completed the entire two-way crossover trial. Both groups received local topical instillation three to four times daily. After four weeks of treatment and control measures, the groups were crossed over and treated for another four weeks. The results showed that the burning sensation was significantly lower in the hyaluronic acid group than in the polyvinyl alcohol group, and the recovery of corneal function was better in the hyaluronic acid group than in the polyvinyl alcohol group (P = 0.04 < 0.05).
Kératite: Liu Jun [27] a publié en 2011 un essai clinique contrôlé randomisé sur le traitement de la kératite du virus de l’herpès simplex avec de l’acide hyaluronique. Au total, 26 sujets ont été inclus, dont 14 dans le groupe traité et 12 dans le groupe témoin. Les mesures de traitement pour le groupe de traitement étaient:0,1% acide hyaluronique gouttes pour les yeuxLe groupe témoin a reçu des gouttes pour les yeux de Tylenol associées au ganciclovir. Les résultats ont montré que les gouttes ophtalmiques à l’acide hyaluronique pourraient raccourcisser le temps de guérison épithéliale et améliorer l’acuité visuelle chez les patients atteints de kératite épithéliale herpès simplex.
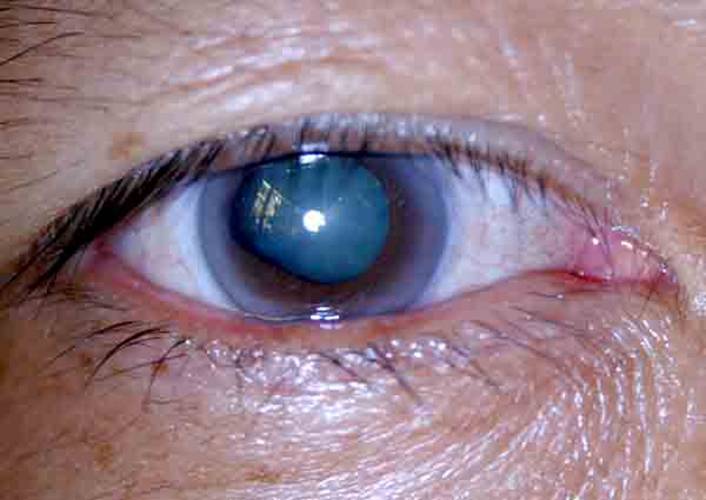
Low intraocular pressure: Kucukerdonmez et al. [28] conducted a clinical study on the treatment of chronic low intraocular pressure with hyaluronic acid, enrolling 32 patients with low intraocular pressure, with an average age of 56.8 years. The treatment involved intravitreal injection of sodium hyaluronate. After treatment, patients recovered well, indicating that hyaluronic acid is effective for treating low intraocular pressure.
Eye burns: Zhao Fajun et al. [29] treated patients with eye burns using traditional methods such as erythromycin or tetracycline eye ointment, chloramphenicol eye drops, and atropine for mydriasis when necessary. Additionally, they administered 0.1% sodium hyaluronate eye drops combined with 2% ofloxacin eye drops every 4 hours. Results showed that early application of sodium hyaluronate after eye burns reduced severe complications and disability rates.
2.5 autres
Ye Shufen [30] and Lai Hanbiao et al. [31] reported that the use of hyaluronic acid gel after dental implant surgery effectively reduces pain responses and alleviates redness and swelling. Wu et al. [32] and Wang Jianping et al. [33] found that hyaluronic acid administered to patients after dacryocystitis surgery promotes the recovery of lacrimal sac function and reduces postoperative scarring.
Références:
[1]Karen LG, Paul B. acide hyaluronique [J]. Drugs, 1994, 47(3): 536-566.
[2]Liu Zhengping, Wang Bing. Progrès de la recherche clinique sur l’acide hyaluronique [J]. Food and Medicine, 2006, 8(12A): 8-10.
[3]Weissmann B, Meyer K. la structure de l’acide hyalobiuronique et de l’acide hyaluronique du cordon ombilical [J]. J Am Chem Soc, 1954, 76(7): 1753-1757.
[4]Cui, Yuan, Duan, Qian, et Li, Yanhui. Progrès de la recherche sur l’acide hyaluronique [J]. Journal of Changchun University of Science and Technology: Natural Science Edition, 2011, 34(3): 101-106.
[5] Liu L,Liu Y,Li J,et al.production microbienne de l’acide hyaluronique: état actuel, défis et perspectives[J]. Microb Cell Fact,2011,10(99) : 1 — 9. La politique
[6] Iannitti T,Lodi D,Palmieri b.injections intra-articulaires pour le traitement de l’arthrose: focus sur l’utilisation clinique de l’acide hyaluronique [J]. Drugs R D,2011,11(1) : 13-27.
[7]Wobig M,Dickhut A,Maier R, et al.viscosupplémentation avec Hylan G - F 20: essai contrôlé de 26 semaines sur l’efficacité et l’innocuité du genou ostéoarthritique [J]. Clin Terapeut,1998,20(3) : 410-423.
[8] Jean Brandt KD, bloc JA,Michalski JP. efficacité and safety De intraarticulaire Hyaluronate de sodium dans l’arthrose du genou [J]. Clin orthoped connexes Res, 2001,385: 130 -143.
[9] Bannuru RR, Natovz NS,Dasi UR, et al.trajectoire thérapeutique suite à l’injection d’acide hyaluronique intra-articulaire dans l’arthrose du genou E méta - Analyse [J]. Osteoarthritis and Cartilage,2011,19(6) : 611-619.
[10] Manfredini D,Piccotti F,Guarda-Nardini L.Hyaluronic acid in the treatment of TMJ disorders: a systematic review of the literature[J]. The Journal of Craniomandibular Practice,2010,28(3) : 166 -176.
[11]Loveday D,Clifton R, Robinson A.Interventions pour traiter les défauts ostéochondriques du talus chez les adultes [J]. Base de données Cochrane de rapports systématiques, publié en ligne: août 2010. DOI: 10.1002/14651858. CD00 8104.
[12] Saito S,Furuya T,Kotake s.effets thérapeutiques des injections d’hyaluronate chez les patients souffrant de douleurs chroniques à l’épaule: une méta-analyse d’essais contrôlés randomisés [J]. Arthritis Care and Research,2010,62(7) : 1 009 - 1 018.
[13] Teh BM,Shen Y,Friedland PL,et Au niveau régionalreview on the use of hyaluronic Acide dans la cicatrisation de la blessure de la membrane tympanique [J]. Expert Opin Biol Ther, 2012,12(1) : 23-36.
[14] Dover JS,Rubin MG,Bhatia ac.examen des données sur l’efficacité, la durabilité et l’innocuité de deux agents de charge d’acide hyaluronique stabilisés non animaux provenant d’une étude Prospective, randomisée,Comparative et multicentrique [J]. Dermato — logic Surgery,2009,35(1) : 322-331.
[15] Stegmann R, Miller D. utilisation of Hyaluronate de sodium dans Traumatisme oculaire pénétrant grave [J]. Ann Ophthalmol,1986,18(1) : 9 -13.
[16]Voigt J, pilote VR. Dérivés d’acide hyaluronique et leur effet curatif sur les brûlures, épithéliales surgical Blessures, et chronic Plaies: a systematic review and méta-analyse of randomisé controlled trials [J]. Wound Repair and Regeneration,2012,20(3) : 317 -331.
[17] Metwally M,Gorvy D,Watson A,et al.Hyaluronic Agents fluides acides pour la La prévention of adhesions after Préservation de la fertilité-préservation Chirurgie gynécologique: une méta-analyse d’essais contrôlés randomisés [J]. Fertility and Sterility,2007,87(5) : 1 139 -1 146.
[18] Mais V,Cirronis MG,Peiretti M,et al. Efficacité de Auto-crosslinked hyaluronan gel for adherence prevention in laparoscopy and hysteroscopy: a systematic review and meta-analysis of randomisation controlled trials[J]. European Journal of Obstetrics and Gynecology and Reproductive Biolo- gy,2012,160(1) : 1-5.
[19] Gupta AK,Paquet M,Villanueva E,et al.Interventions for actinic ker- atoses[J]. Base de données Cochrane des revues systématiques, publiée en ligne: 2012 décembre. DOI: 10.1002/14651858.CD004415.
[20]Kirova YM,Fromantin I,De Rycke Y,et al. action in breast cancer patients using hyaluronic acid Pendant le rayonnement Thérapie? Résultats obtenus of phase III randomised Procès [J]. radiautre Oncol, 2011,100(2) : 205-209.
[21]Pinnix C,Perkins GH,Strom EA,et 1. Topique Hyaluronic Acide vs.Standard of Soin de la prévention of Radiation Dermatite après Adjuvant radiothérapie for sein Cancer: Simple - aveugle Essai clinique randomisé de Phase III [J]. International Journal of Radiation Oncology Biology Physics,2012,83(4) : 1 089 -1 094.
[22] Yu Chunshui, Ran Liwei, Tan Shengshun et al. Analyse de l’efficacité de l’injection locale d’hyaluronate de sodium et d’hyaluronidase dans le traitement de la sclérodermie localisée au stade avancé [J]. Chinese Journal of Dermatology, 2006, 20(1): 26-28.
[23] Narins RS,Brandt F,Leyden J,et al. Une comparaison randomisée, en double aveugle et multi-ticenter de l’efficacité et de la tolérabilité de Restylane versus Zy- plast pour la correction des plis nasolabiaux [J]. Chirurgie dermatologique: publication officielle pour les Société pour dermatologique Chirurgie,2003, 29(6) : 588-595.
[24] Algawi K,Agrell B,Goggin M,et al.essai clinique randomisé de topique Hyaluronate de sodium après kératectomie photoréfractive au laser excimère [J]. J Refract Surg,1995,11(1) : 42-44.
[25] Faraldi F,Papa V,Santoro D,et al.A Nouveau: eye gel Contenant: sodium hyaluronate and Le xanthane gomme for the La gestion Des abrasions cornéennes post-traumatiques [J]. Journal of Clinical Ophthalmology,2012,6: 727 - 731.
[26] McDonald CC,Kaye SB,Figueiredo FC,et al.A randomisé,crossover, multicentrique study to compare the La performance of 0.1% (w/v) sodium hyaluronate with 1,4% (w/v) Alcool polyvinylique dans l’atténuation de Symptômes associés au syndrome de l’œil sec [J]. Eye (londres, Angleterre), 2002,16(5) : 601-607.
[27]Liu Jun. Effect of sodium hyaluronate eye drops on epithelial healing in herpès simplex virus kératite [J]. Huaihai Medicine, 2011, 29(6): 522-523.
[28]Kucukerdonmez C, Beutel J, Bartz-Schmidt KU, et al. Traitement de l’hypotonie oculaire chronique par application intraoculaire d’hyaluronate de sodium [J]. British Journal of Ophthalmology, 2009, 93(2): 235-239.
[29]Zhao Fajun, Zong Xiao. Observation sur l’efficacité de l’hyaluronate de sodium dans le traitement des brûlures chimiques de l’oeil [J]. Medical Theory and Practice, 2007, 20(1): 69-70.
[30]Ye Shufen. Le rôle du gel d’acide hyaluronique GENGIGEL® dans la cicatrisation des plaies après la chirurgie d’implant [J]. International Journal of Medicine and Health, 2006, 12(7): 34-35.
[31]Lai Han-Biao, Liu Yi. Le rôle du gel d’acide hyaluronique dans la cicatrisation des plaies après la chirurgie d’implant [J]. Guangdong Journal of Stomatology, 2008(16): 637-638.
[32]Wu W, Cannon PS, Yan W, et al. Effets de la couverture de mérogel sur la cicatrisation des plaies et la patence ostiale dans la dacryocystorhinostomie endoscopique endonasale pour la dacryocystite chronique primaire [J]. Eye (Lond), 2011, 25(6): 746-753.
[33]Wang Jianping, Zhang Deshou, Ma Yong, et al. Application d’hyaluronate de sodium dans l’anastomose nasolacrimal [J]. International Journal of Ophthalmology, 2009, 24(6): 3828-3829.
-
Précédent précédent
Quelles sont les utilisations de la poudre d’acide hyaluronique dans l’arthrose?
-
Suivant:
Quelles sont les utilisations de la poudre d’acide hyaluronique dans le domaine alimentaire?


 Anglais
Anglais français
français espagnol
espagnol russe
russe coréen
coréen japonais
japonais